Structure and Composition of Periodontal Ligament
- PDL consists of principal fibres, loose connective tissue, blast and clast cells, oxytalan fibres, and Cell Rest of Malassez.
- Alveolodental ligament is the main principal fiber group, consisting of five fiber subgroups: alveolar crest, horizontal, oblique, apical, and interradicular.
- Transseptal fibers are principal fibers other than the alveolodental ligament.
- Alveolar crest fibers run from the cervical part of the root to the alveolar bone crest.
- Horizontal fibers attach to the cementum apical to the alveolar crest fibers and run perpendicularly from the root to the alveolar bone.
- PDL substance is estimated to be 70% water, affecting the tooth's ability to withstand stress loads.
- PDL ranges in width from 0.15 to 0.38mm, thinnest in the middle third of the root.
- PDL is part of the periodontium that attaches teeth to the surrounding alveolar bone via cementum.
- PDL appears as a radiolucent area between the lamina dura and cementum on radiographs.
- Completeness and vitality of the PDL are essential for tooth functioning.
Development and Effects of Mechanical Forces on Periodontal Ligament
- PDL cells are derived from the dental follicle after crown formation and root development.
- Formation of PDL starts at the cementoenamel junction and progresses apically.
- Movement of teeth involves deposition of bone on the tension side and resorption on the compression side of the PDL.
- Fibroblasts in the PDL react to mechanical stress, affecting osteoblastogenesis and osteoclastogenesis.
- Mechanical stimuli can lead to differentiation of osteocytes into osteoclasts, remodeling the bone structure.
- Orthodontic treatment applies mechanical force to align teeth, involving physical and cellular processes.
Function of Periodontal Ligament
- PDL functions include support, sensory perception, nutrition, and remodeling.
- PDL provides attachment between teeth and alveolar bone, absorbing and transmitting forces during mastication.
- PDL is heavily innervated, involving mechanoreception, nociception, and reflexes.
- PDL maintains vitality of surrounding cells through anastomosed blood vessels.
- Progenitor cells in the PDL can differentiate into osteoblasts for maintenance and repair of alveolar bone.
Clinical Significance of Periodontal Ligament
- Traumatic forces of occlusion can cause widening of the PDL space, seen on radiographs.
- PDL damage may result in tooth ankylosis and pathological tooth migration.
- PDL cells of an avulsed tooth are at risk of drying and desiccation, affecting replantation success.
- Early occlusal trauma can manifest as increased tooth mobility.
- Subluxation may cause tearing of the PDL and pain during function.
Additional Topics
- Effect of tobacco smoking and nicotine on periodontal health.
- Ankylosis and its causes.
- Effect of nutrition on periodontal tissues, including the role of vitamins D and C.
Note: The "See also" section and the references have been excluded from the groups as they do not contain additional content to be organised.
The periodontal ligament, commonly abbreviated as the PDL, is a group of specialised connective tissue fibers that essentially attach a tooth to the alveolar bone within which it sits. It inserts into root cementum on one side and onto alveolar bone on the other.
| Periodontal ligament | |
|---|---|
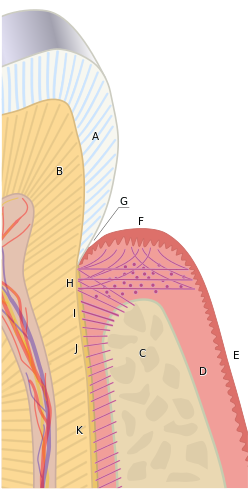 The tissues of the periodontium combine to form an active, dynamic group of tissues. The alveolar bone (C) is surrounded for the most part by the subepithelial connective tissue of the gingiva, which in turn is covered by the various characteristic gingival epithelia. The cementum overlaying the tooth root is attached to the adjacent cortical surface of the alveolar bone by the alveolar crest (I), horizontal (J) and oblique (K) fibers of the periodontal ligament. | |
| Details | |
| Precursor | dental follicle |
| Identifiers | |
| Latin | fibra periodontalis |
| Acronym(s) | PDL |
| MeSH | D010513 |
| FMA | 56665 |
| Anatomical terminology | |