Signs, Symptoms, and Diagnosis
- Protrusive growth at the mandible or maxilla
- Facial asymmetry due to cyst expansion
- Impact at the anterior region of mandible
- Painful and swollen sensation at the jaw region
- Root resorption, cortical bone thinning, and tooth displacement
- BCL-2 protein inhibits apoptosis and may contribute to GOC development
- Traumatic events can lead to GOC formation
- Mutated cells from oral mucosa and dental follicle may cause GOC
- Pre-existing cysts or cancerous constituents can be a probable cause
- GOC can originate from a salivary gland or simple epithelium
- Computed tomography is essential for imaging
- GOC may appear unilocular or multilocular
- Prevalence of GOC at the upper jaw is 71.8%
- Scalloped margin surrounding the GOC
- Average size of GOC is 4.9cm
- Stratified squamous epithelium attached to connective tissue
- Non-keratinised lining with inconsistent diameter
- Basal cells not associated with cancerous origin
- Increased calcium concentration can cause calcification
- Presence of eosinophilic organelles and intra-epithelial crypts
- Differential diagnosis includes central mucoepidermoid carcinoma, odontogenic keratocyst, ameloblastoma, odontogenic myxoma, and dentigerous cyst
Immunocytochemistry and MAML2 Rearrangement
- Cytokeratin profiles can differentiate between GOC and central MEC
- GOC and central MEC show individualised expression for cytokeratin 18 and 19
- Ki-67, p53, and PCNA expression observed in common jaw cysts
- Lack of p53 expression found in radicular cysts
- Ki-67 expression lower in central MEC compared to other lesions
- MAML2 rearrangement useful in differential diagnosis of GOC and central MEC
- CRTC3-MAML2 fusion observed in a second cystic development
- MAML2 rearrangement represents the growth of central MEC from GOC
- Fusion-gene transcript helpful in differentiating GOC from central MEC
- MAML2 rearrangement observed in jaw and salivary gland lesions
Treatment
- Enucleation
- Curettage
- Marginal or partial resection
- Marsupialization
- Follow-up post-surgery to prevent recurrence
- Pre-treatment protocols involve panoramic radiography and computed tomography
- Scans provide information on GOC size, radiolucency, cortical bone, etc.
- Dentition may be embedded in cavity walls depending on expansion position
- Smaller GOCs attached to two teeth, larger GOCs attached to more teeth
- Greater sised lesions require biopsy and precise treatment plan
- Unilocular GOCs with minimal tissue deterioration can be treated with enucleation, curettage, and marsupialization
- Enucleation or curettage may be incomplete for less invasive lesions
- Multilocular GOCs require peripheral ostectomy, marginal resection, or partial jaw resection
- Marsupialization recommended for GOCs with severe structural damage
- Dredging method (repetition of enucleation and curettage) may be necessary
- Follow-up appointments necessary due to high chance of remission
- Remission rate of 21 to 55% within 0.5 to 7 years post-surgery
- Lower risk lesions require appointments for up to 3 years post-surgery
- Higher risk lesions require appointments for up to 7 years post-surgery
- Remission events require appropriate procedures such as enucleation or curettage
Definition, Characteristics, and Clinical Presentation
- A benign cystic lesion that arises from odontogenic epithelium
- Most commonly occurs in the mandible
- Predominantly affects adults, with a slight male predilection
- Often asymptomatic and discovered incidentally on radiographic examination
- Histologically characterised by the presence of gland-like structures and cuboidal/columnar epithelium
- Frequently presents as a painless swelling or a radiolucency on imaging
- May cause cortical expansion and displacement of adjacent teeth
- Diagnosis is confirmed through histopathological examination of a biopsy specimen
- Differential diagnosis includes other odontogenic cysts and tumors
- Radiographic features may include well-defined borders and scalloping of adjacent roots
Complications, Associated Conditions, and Research
- Potential complications include infection, fracture, and displacement of adjacent structures
- Glandular odontogenic cysts have been associated with other odontogenic lesions, such as ameloblastoma and mucoepidermoid carcinoma
- Rare cases of malignant transformation have been reported
- Recurrence of the cyst may occur if not adequately treated
- Long-standing cysts may lead to bone resorption and loss of teeth
- Studies have investigated the expression of specific markers, such as podoplanin and TGF-beta, in glandular odontogenic cysts
- Molecular analysis, such as MAML2 rearrangement, can help confirm the diagnosis of central mucoepidermoid carcinoma arising from a glandular odontogenic cyst
- Research has focused on the diagnostic challenges and dilemmas associated with glandular odontogenic cysts
- Treatment modalities and outcomes have been studied to improve patient management
- Further research is needed to better understand the pathogenesis and molecular characteristics of glandular odontogenic cysts.
A glandular odontogenic cyst (GOC) is a rare and usually benign odontogenic cyst developed at the odontogenic epithelium of the mandible or maxilla. Originally, the cyst was labeled as "sialo-odontogenic cyst" in 1987. However, the World Health Organization (WHO) decided to adopt the medical expression "glandular odontogenic cyst". Following the initial classification, only 60 medically documented cases were present in the population by 2003. GOC was established as its own biological growth after differentiation from other jaw cysts such as the "central mucoepidermoid carcinoma (MEC)", a popular type of neoplasm at the salivary glands. GOC is usually misdiagnosed with other lesions developed at the glandular and salivary gland due to the shared clinical signs. The presence of osteodentin supports the concept of an odontogenic pathway. This odontogenic cyst is commonly described to be a slow and aggressive development. The inclination of GOC to be large and multilocular is associated with a greater chance of remission. GOC is an infrequent manifestation with a 0.2% diagnosis in jaw lesion cases. Reported cases show that GOC mainly impacts the mandible and male individuals. The presentation of GOC at the maxilla has a very low rate of incidence. The GOC development is more common in adults in their fifth and sixth decades.
| Glandular odontogenic cyst | |
|---|---|
| Other names | Sialo-Odontogenic cyst |
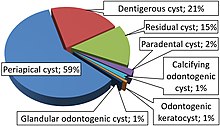 | |
| Relative incidence of odontogenic cysts. Glandular odontogenic cyst is labeled at bottom. | |
| Symptoms | Jaw expansion, swelling, impairment to the tooth, root and cortical plate |
| Causes | Cellular mutation, cyst maturation at glandular, BCL-2 protein |
| Diagnostic method | Biopsy, CT scans, Panoramic x-rays |
| Differential diagnosis | Central mucoepidermoid carcinoma, odontogenic keratocyst |
| Prevention | Post-surgery follow-ups are commonly proposed to prevent the chances of recurrence |
| Treatment | Enucleation, curettage, marginal or partial resection, marsupialization |
| Frequency | 0.12 to 0.13% of people |
GOC has signs and symptoms of varying sensitivities, and dysfunction. In some cases, the GOC will present no classic abnormalities and remains undiagnosed until secondary complications arise. The proliferation of GOC requires insight into the foundations of its unique histochemistry and biology. The comparable characteristics of GOC with other jaw lesions require the close examination of its histology, morphology, and immunocytochemistry for a differential diagnosis. Treatment modes of the GOC follow a case-by-case approach due to the variable nature of the cyst. The selected treatment must be accompanied with an appropriate pre and post-operative plan.