Coagulation Process
- Vasoconstriction: Endothelial cells release vasoconstrictor substances like endothelin and thromboxane, reducing blood flow to the site of injury.
- Platelet activation and platelet plug formation: Platelets bind to collagen, release granules containing ADP, serotonin, and thromboxane A2, and form a platelet plug.
- Coagulation cascade: Two pathways (contact activation and tissue factor) lead to fibrin formation and the formation of a stable blood clot.
- Fibrin clot formation: Thrombin converts fibrinogen into fibrin, which forms a clot that temporarily seals the wound.
- Hemostasis stages: Vasoconstriction, platelet activation and plug formation, coagulation cascade, fibrin clot formation, and clot retraction and resolution.
Coagulation Factors
- Coagulation factors are enzymes called serine proteases.
- Tissue factor, FV, FVIII, and FXIII have different structures and are exceptions to the serine protease rule.
Coagulation Pathways
- Tissue Factor Pathway (Extrinsic): TF-FVIIa complex activates FIX and FX, leading to thrombin burst and fibrin formation.
- Contact Activation Pathway (Intrinsic): FXIIa converts FXI into FXIa, which activates FIX and forms the tenase complex.
- Final Common Pathway: Thrombin converts prothrombin to thrombin, which converts fibrinogen to fibrin, activates Factors VIII and V, and forms crosslinks in fibrin polymers.
Role in Immune System and Cofactors
- Coagulation system physically traps microbes, increases vascular permeability, and acts as chemotactic agents for phagocytic cells.
- Calcium, phospholipids, and vitamin K are required for coagulation factor complexes and their functions.
Medical Assessment and Role in Disease
- Medical tests assess coagulation system function, including aPTT, PT, fibrinogen testing, platelet count, and platelet function testing.
- Coagulation defects can cause hemorrhage or thrombosis, and platelet and coagulation factor disorders can lead to bleeding or impaired clotting.
- Pharmacology: Procoagulants, anticoagulants, and their uses in various medical conditions.
- History: Theories, discoveries, and nomenclature related to coagulation factors.
Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The mechanism of coagulation involves activation, adhesion and aggregation of platelets, as well as deposition and maturation of fibrin.
| Coagulation | |
|---|---|
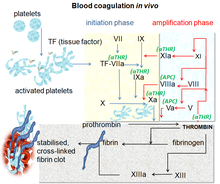 Blood coagulation pathways in vivo showing the central role played by thrombin | |
| Health | Beneficial |
Coagulation begins almost instantly after an injury to the endothelium lining a blood vessel. Exposure of blood to the subendothelial space initiates two processes: changes in platelets, and the exposure of subendothelial tissue factor to plasma factor VII, which ultimately leads to cross-linked fibrin formation. Platelets immediately form a plug at the site of injury; this is called primary hemostasis. Secondary hemostasis occurs simultaneously: additional coagulation (clotting) factors beyond factor VII (listed below) respond in a cascade to form fibrin strands, which strengthen the platelet plug.
Disorders of coagulation are disease states which can result in problems with hemorrhage, bruising, or thrombosis.
Coagulation is highly conserved throughout biology. In all mammals, coagulation involves both cellular components (platelets) and proteinaceous components (here, coagulation factors). The pathway in humans has been the most extensively researched and is the best understood.
Borrowed from Middle French coagulation, from Latin coagulatio, coagulationem. Morphologically coagulate + -ion
coagulation (countable and uncountable, plural coagulations)